The integration of Artificial Intelligence (AI) diagnostics and decision support systems into healthcare workflows has the potential to significantly enhance clinical outcomes worldwide. This integration, particularly critical in resource-limited settings, demands careful consideration to ensure accuracy and build clinician trust across diverse health systems.
1. Effective Methods for Integration
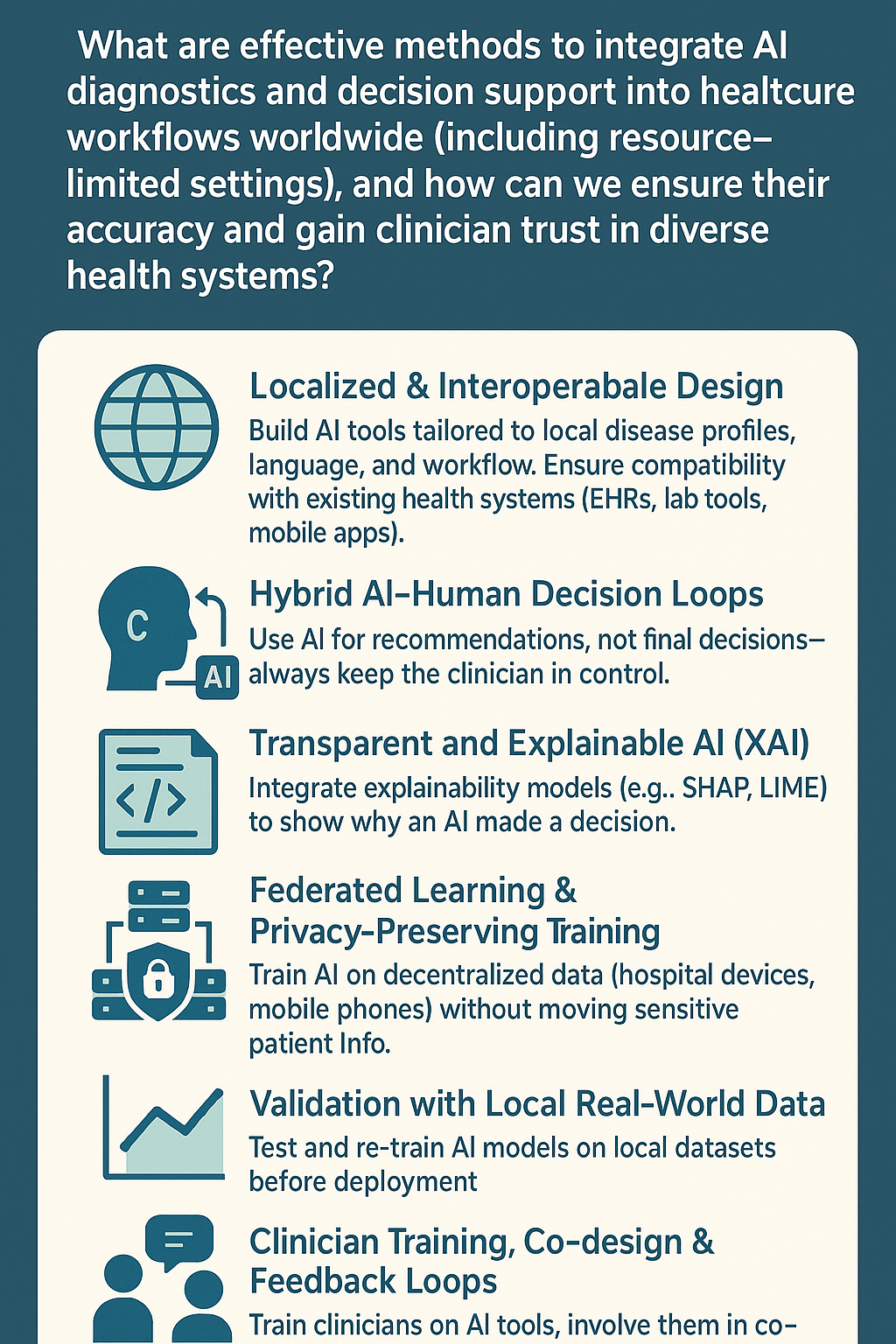
To effectively embed AI solutions into healthcare workflows:
- Workflow Alignment: AI tools must seamlessly integrate into existing clinical processes without adding complexity. User-friendly interfaces and clear integration into Electronic Health Records (EHRs) facilitate ease of adoption.
- Clinician Engagement: Involving healthcare providers from the development phase ensures AI tools meet actual clinical needs and workflow realities.
- Capacity Building and Training: Comprehensive training programs equip clinicians with the knowledge to interpret AI-generated insights confidently.
2. Adapting to Resource-Limited Settings
Resource-constrained environments present unique integration challenges. Effective strategies include:
- Low-Resource AI Solutions: Designing AI models that require minimal computational resources and can operate offline or on mobile devices.
- Frugal Innovation: Leveraging open-source platforms and locally available technology infrastructures to deploy affordable AI solutions.
- Telemedicine Integration: Combining AI diagnostics with telehealth platforms to extend reach into remote and underserved regions.
3. Ensuring Accuracy and Reliability
Accuracy and reliability of AI diagnostic tools can be enhanced by:
- Robust Data Training: Utilizing diverse datasets representative of various demographics and clinical conditions to train and validate AI algorithms.
- Continuous Monitoring and Updates: Implementing real-time performance monitoring and regular algorithm retraining based on emerging clinical data.
- Transparent AI Models: Adopting explainable AI (XAI) approaches that allow clinicians to understand the reasoning behind AI recommendations, fostering trust and accountability.
4. Gaining Clinician Trust
Clinician trust is paramount for the successful adoption of AI tools:
- Transparency and Interpretability: Clear communication of AI functionality, strengths, and limitations helps clinicians make informed decisions.
- Evidence-Based Validation: Rigorous, peer-reviewed studies and real-world trials demonstrating clinical effectiveness and safety build credibility.
- Collaborative Decision Making: AI should complement, not replace, clinical judgment, emphasizing its role as a supportive tool rather than a substitute.
5. Regulatory and Ethical Considerations
To foster trust and ensure safe integration:
- Ethical Standards: Adhering to internationally accepted ethical frameworks, protecting patient data privacy, and addressing potential biases in AI algorithms.
- Regulatory Compliance: Complying with region-specific healthcare regulations and global standards to ensure consistency and reliability.
6. Successful Examples of Global AI Integration
- AI-powered Imaging: Deep learning algorithms in radiology and pathology have been successfully integrated into diagnostic workflows in both developed and developing countries.
- AI-based Clinical Decision Support (CDS): Systems providing real-time decision support in critical care settings, such as sepsis detection, have shown to significantly improve patient outcomes.
Conclusion
Integrating AI into healthcare workflows worldwide involves strategic alignment, robust technology adaptation for resource-constrained environments, consistent accuracy validation, and transparent engagement with clinicians. Building trust through transparency, evidence-based validation, and ethical compliance will be crucial to harnessing AI’s full potential in healthcare globally.